September 12, 2024
Management Of Urinary Incontinence In Postmenopausal Ladies: An Emas Clinical Overview
Monitoring Of Urinary System Incontinence In Postmenopausal Females: An Emas Medical Overview [23] is entitled the partnership in between menopause and urinary incontinence that females with urinary system incontinence than those that did not have, significantly had greater BMI [24] Medical care professionals must consider urinary system incontinence a clinical priority and develop suitable diagnostic abilities. They need to have the ability to identify and take care of any type of relevant modifiable aspects that can ease the problem. Later on, in a subgroup of these people, myopathic modifications may occur in the bladder that make the spread of extraordinarily generated contractile signals extra efficient and more difficult to reduce willingly. These connective-tissue elements form the passive sustains to the urethra and bladder neck. During times of raised intra-abdominal pressure, if these supports are intact, they increase the helpful effect of muscle closure of the pelvic flooring. INNOVO's distinct Multipath ™ Innovation ensures optimum muscle interaction and efficacy, providing targeted stimulation to the pelvic flooring muscles without the requirement for invasive probes or hand-operated intervention.
List Of Reduced Estrogen Bladder Symptoms
Because of the position and feature of steroids in the urinary tract, making use of replaced hormone treatment in menopause has long drawn in the attention of researchers and suppliers of healthcare in this area. In ladies without urethral hypermobility, the urethra is stabilized during stress and anxiety by three related mechanisms. One system is response, or volunteer, closure of the pelvic floor. Tightening of the levator rectum facility elevates the proximal urethra and bladder neck, tightens undamaged connective cells supports, and raises the perineal body, which might serve as a urethral backstop. If you're experiencing urinary incontinence during your duration or your cycle, it can transform your lifestyle.Neurologic Reasons
In 1989, the National Institutes of Health And Wellness Consensus Development Seminar approximated the yearly Cloudy urine expense of urinary system incontinence in the USA to be $12.4 billion. Real expenses can be tough to estimate because lots of people do not come to the focus of medical experts. Urinary system urinary incontinence should not be thought of as a disease, because no specific etiology exists; most individual situations are most likely multifactorial in nature. The etiologies of urinary system incontinence vary and, in a lot of cases, incompletely comprehended. It is essential to inform your doctor or registered nurse if you are having troubles.How Can I Decrease My Danger Of Stress Urinary Incontinence?
During this procedure, the posterior wall of the urethra shears off the anterior urethral wall surface to open up the bladder neck when innate sphincter shortage is present. Practical urinary incontinence is the failure to hold urine as a result of factors besides neuro-urologic and lower urinary system tract dysfunction. Videourodynamic studies are reserved to evaluate intricate situations of stress and anxiety urinary incontinence.- The psychosocial prices and morbidities are much more challenging to quantify.
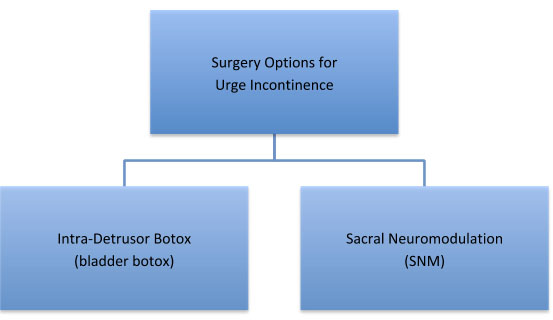
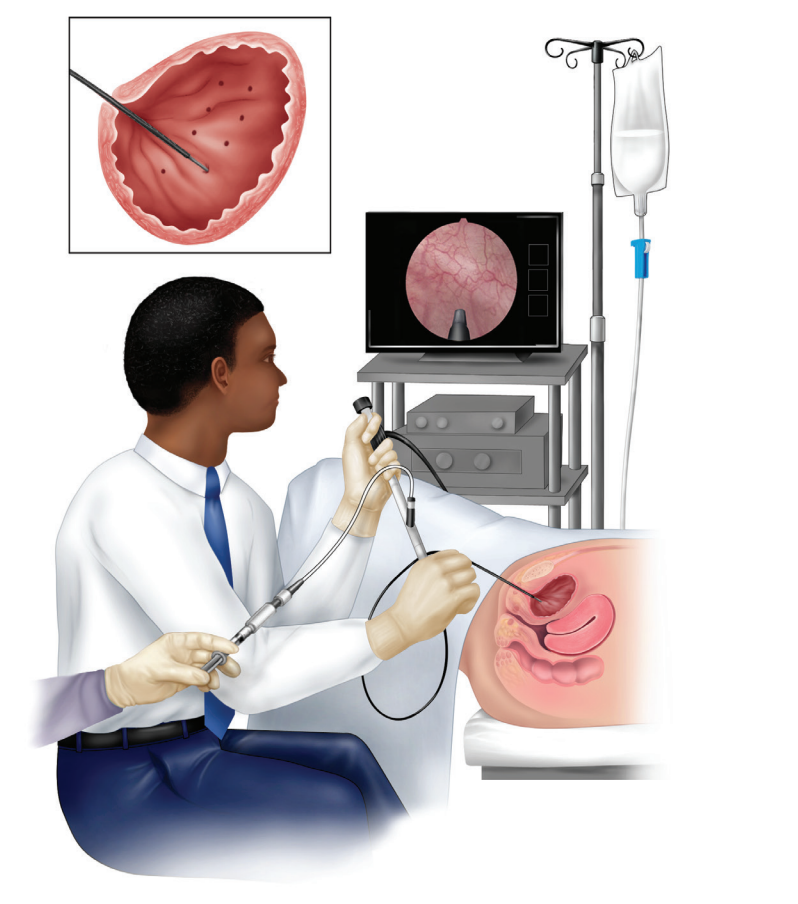
- Your healthcare provider might advise repeating the injections once or twice a year.
- If other approaches for aiding stress incontinence do not function, your doctor could recommend surgical procedure.
- One of the most typical hereditary disorders creating incontinence consist of ectopic ureter( s), and relevant anatomic abnormalities (license urachus, pseudohermaphrodites, and urethrorectal fistulae).
What hormone maintains you from peeing?
Social Links